Breast cancer screening is a vital tool in the early detection and management of breast cancer, significantly impacting outcomes by identifying the disease at an earlier, more treatable stage. This blog post aims to unpack the multifaceted aspects of breast cancer screening, from its rationale and the identification of risk groups to the various screening modalities and the emerging role of artificial intelligence (AI), as well as a glimpse into the future of breast cancer detection.
The Rationale for Screening
The primary rationale for breast cancer screening is early detection. Studies have consistently shown that finding breast cancer early reduces mortality from the disease by providing a chance to treat it before it spreads. Early-stage breast cancers often have more treatment options and a better prognosis than those diagnosed at a later stage.
Identifying Risk Groups
Breast cancer risk is not uniform across the population; it varies based on genetic, environmental, and lifestyle factors. Understanding these risk factors is crucial for tailoring screening recommendations.
- Average Risk: Women without a personal or strong family history of breast cancer, no genetic predisposition, and no previous radiation therapy to the chest before the age of 30 fall into the average-risk category. Typically, this group is recommended to start mammography screening at age 40 to 50, depending on the guidelines followed.
- High Risk: Individuals are considered at high risk if they have a known BRCA1 or BRCA2 gene mutation, a family history suggestive of a genetic predisposition, a personal history of breast cancer or certain non-cancerous breast diseases, or they received radiation therapy to the chest during childhood or early adulthood. High-risk individuals may need to start screening earlier, often before the age of 40, and may require additional screening modalities such as MRI.
Screening Modalities and Their Pros and Cons
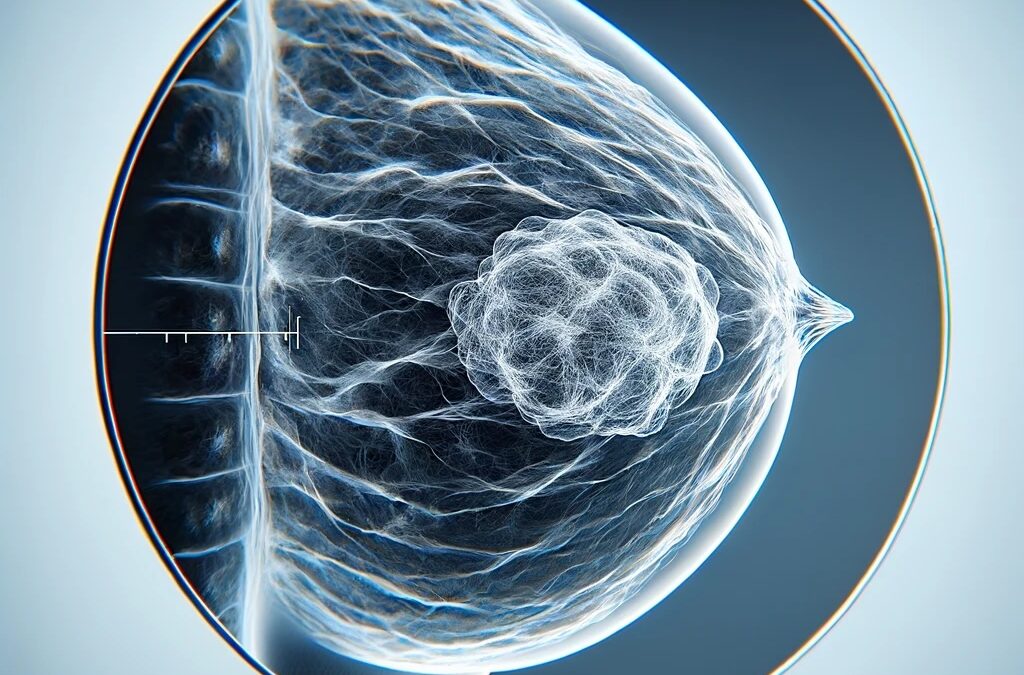
- Mammography: The cornerstone of breast cancer screening, mammography can detect tumors before they are palpable. The primary advantage of mammography is its widespread availability and proven effectiveness in reducing breast cancer mortality. However, it has limitations, such as false positives, false negatives, and the potential for overdiagnosis.
- MRI: Breast MRI offers a more sensitive screening option for high-risk individuals, capable of detecting cancers missed by mammography. Its downside includes higher costs, limited availability, and a higher rate of false positives, leading to unnecessary biopsies in some cases.
- Ultrasound: Often used as a complementary tool, especially in women with dense breast tissue where mammograms are less effective. Ultrasound can help distinguish between solid masses and fluid-filled cysts. Its limitations include operator dependency and a higher chance of false positives.
Advances in Breast Cancer Screening
The field of breast cancer screening is on the cusp of significant advancements, promising to enhance early detection, improve accuracy, and offer more personalized approaches to care. These innovations are driven by technological advancements, deeper understanding of genetic factors, and a push towards minimally invasive techniques. Here’s a look at some of the recent advances that are expected to shape the future of breast cancer screening over the next decade:
1. Artificial Intelligence and Machine Learning
Artificial Intelligence (AI) and Machine Learning (ML) technologies are set to transform breast cancer screening by increasing the accuracy and efficiency of mammogram analysis. AI algorithms can detect subtleties in imaging that may be overlooked by the human eye, reducing false negatives and identifying cancers at earlier stages. Moreover, AI can help in minimizing false positives, thereby decreasing unnecessary anxiety and invasive follow-up procedures. Continuous improvement in AI algorithms, fueled by larger datasets and more sophisticated neural networks, will further refine screening accuracy and reliability.
2. Advanced Imaging Technologies
- Digital Breast Tomosynthesis (DBT): Also known as 3D mammography, DBT creates a three-dimensional image of the breast, improving the detection of small tumors and reducing the impact of overlapping breast tissue, a common issue in traditional 2D mammography, especially in women with dense breasts.
- Contrast-Enhanced Mammography (CEM): CEM combines mammography with intravenous contrast medium to highlight blood vessels and lesions that may not be visible on standard mammograms, offering another tool for early detection, especially in dense breasts.
3. Molecular Breast Imaging (MBI)
MBI is a nuclear medicine technique that detects tumors based on their metabolic activity, rather than their shape or density. It involves the injection of a radioactive tracer that cancer cells absorb more than normal cells, making it a highly sensitive tool for detecting small lesions in dense breast tissue.
4. Liquid Biopsies and Biomarkers
The development of liquid biopsies, which detect cancer cells or DNA in the blood, could revolutionize breast cancer screening by providing a non-invasive method to identify cancers at their earliest stages. Research into specific biomarkers associated with breast cancer is ongoing, and these could eventually be used alongside or as an alternative to traditional imaging methods for screening or monitoring high-risk patients.
5. Genetic Screening and Risk Assessment Tools
Advancements in genetic testing, including more comprehensive panels that go beyond BRCA1 and BRCA2 mutations, are allowing for more precise risk stratification. This, combined with AI-driven risk assessment tools that incorporate genetic, lifestyle, and environmental factors, will enable more personalized screening strategies. Tailored screening schedules and methods can then be developed based on an individual’s specific risk profile.
6. Integrating Wearable Technology
Emerging research into wearable technology for breast health monitoring, such as smart bras equipped with sensors that detect temperature changes or tissue density variations, could offer continuous, non-invasive monitoring options. While still in the early stages of development, these technologies could one day supplement traditional screening methods, especially for those at high risk.
Conclusion
The foreseeable future promises exciting advances in breast cancer screening, driven by a combination of technological innovation, a better understanding of the genetic basis of cancer, and a move towards more personalized medicine. These advancements are poised to improve early detection rates, reduce the burden of unnecessary procedures, and ultimately, save lives by catching cancers at their most treatable stages. As these technologies mature and become integrated into clinical practice, they will undoubtedly advance the field of breast cancer screening, offering hope for more effective management and outcomes for patients worldwide.


Recent Comments