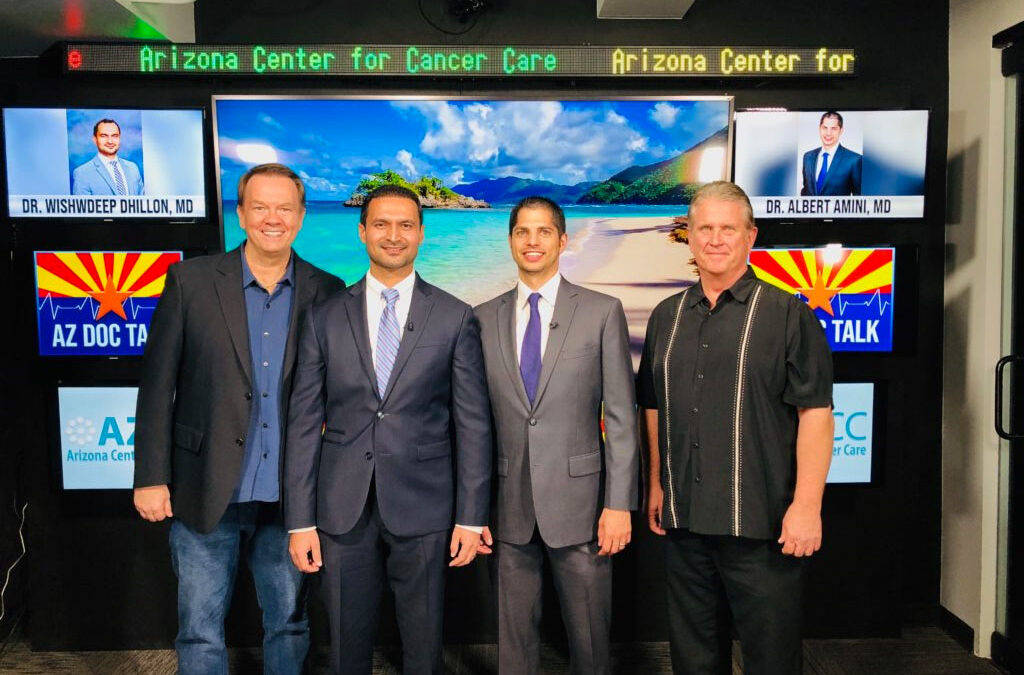
Last month, I got a chance to spend some time with Dr. Albert Amini, Dave Pratt, and Mark Lewis. We talked about different aspects of managing Pancreatic Cancer. Here is a rough transcript of the conversation.
What exactly is the function of the Pancreas?
The Pancreas is a gland in the abdomen that sits behind the stomach and below the liver. It is about 6 inches long. The Pancreas makes essential enzymes that help digest food. These enzymes are emptied into the duodenum through a channel that runs through the Pancreas, called the pancreatic duct. Once in the duodenum, the enzymes help digest the fats, protein, and carbohydrates in food. The Pancreas also makes Insulin hormone, which is essential for the regulation of blood glucose. Finally, the Pancreas serves as a pathway for transport of bile from the liver to the duodenum.
Diseases of the Pancreas can manifest as poor digestion of food, problems with Insulin production or Diabetes, and blockage of bile drainage, which can cause jaundice.
What is the incidence of Pancreatic Cancer compared to other cancers?
Approximately 55000 people in the US are diagnosed with Pancreatic Cancer every year. In the US, about 270000 patients are diagnosed with Breast Cancer each year; around 230000 patients are diagnosed with Lung Cancer each year. Although Pancreatic Cancer is not very common, it is the 4th leading cause of cancer-related death in the US.
What are the causes of Pancreatic Cancer?
Some of the common causes include smoking, heavy alcohol consumption, exposure to chemicals like pesticides, benzene, hydrocarbons, obesity/high BMI, chronic pancreatitis. Having Diabetes also increases the risk of Pancreatic Cancer.
In about 5-10% of cases, Pancreatic Cancer is thought to be caused by genetic or familial factors. Having an affected parent increases the risk of developing Pancreatic Cancer by about five times.
For example, patients with Peutz-Jeghers syndrome and Familial melanoma and pancreatic cancer syndrome have an increased risk of Colorectal cancer (Polyps) and Pancreatic cancer. Familial melanoma and pancreatic cancer syndrome
Lynch Syndrome – caused by mutations in DNA mismatch repair genes – is associated with Colorectal and Pancreatic Cancer
BRCA2 mutation, best known for its association with breast and ovarian cancer, also causes an increased risk of Pancreatic Cancer.
What makes Pancreatic Cancer so dangerous?
There are several reasons for that:
- Pancreatic Cancer is often diagnosed late, which makes surgical resection difficult.
- There are no great screening protocols for Pancreatic Cancer, unlike for example mammograms for breast cancer, or colonoscopy for colon cancer
- Pancreatic Cancer tends to spread early, a process we call micrometastasis. These are cancer cells that may have spread beyond the Pancreas, but we cannot see on scans.
- Pancreatic Cancer cells have this sort of a protective shell of tissue around it that makes it challenging to deliver chemotherapy drugs to the cancer cells
When someone finds out they have Pancreatic Cancer, what should they do?
Pancreatic Cancer is best treated by multidisciplinary teams. The team includes a surgeon, medical oncologist, radiation oncologist, gastroenterologist, and support services like nutrition, genetics, and social services. Finding a team with the right experience who work closely and communicate with each other is the key. As a patient, you have to be comfortable working with your team that provides excellent care but also respects your beliefs and values. Ultimately our patients have to be at the center of everything we do.
When someone is diagnosed with Pancreatic Cancer, should their family members get tested?
Most cases of Pancreatic Cancer are not inherited. However, there may be a genetic basis for Pancreatic Cancer in about 5-10% of cases;
the likelihood may be higher if there are other affected family members with Pancreatic Cancer, Breast Cancer or Ovarian Cancer or Melanoma or Colon Cancer.
In our practice, we recommend genetic testing for all patients with Pancreatic Cancer.
How do you treat Pancreatic Cancer?
After making the diagnosis, staging is an important next step. While evaluating patients for possible surgery, we review the location of the cancer in relation to the blood vessels around the Pancreas. Based on that information, Pancreatic Cancer is labeled “resectable”, “borderline resectable,” and “unresectable”. The treatment of Pancreatic Cancer is evolving. The traditional treatment approach for resectable and borderline resectable Pancreatic Cancer has been surgery followed by chemotherapy with or without radiation. The outcomes with this approach have not been great. Five-year survival after surgery is only approximately 10 percent for node-positive disease, while it is roughly 30 percent for node-negative disease. In fact, after such a major surgery, many patients will not even make it to chemotherapy or radiation on time. We realize that a majority of patients with Pancreatic Cancer who undergo upfront surgery will develop metastatic disease elsewhere, for example, in the liver or lungs. This means that even though we cannot see it at diagnosis, Pancreatic Cancer had already spread to other organs in the form of micrometastatic disease. Therefore upfront surgery is not enough. We need to target the micrometastatic disease early on in the treatment.
In recent years, we have seen a transition towards the so-called “surgery last” approach. When appropriate, we are recommending starting treatment with chemotherapy first. This approach is called neoadjuvant chemotherapy. The intent is to shrink the tumor and increase the chance of a successful resection.
We typically start with a combination of drugs, given on a two weekly basis or weekly basis. The two most commonly used regimens are FOLFIRINOX and Gemcitabine-Nab Paclitaxel.
During treatment, patients may experience diarrhea, fatigue, nausea, hair loss, decreased immunity, neuropathy. Your treatment team will monitor closely for these side effects and make appropriate changes.
We typically repeat scans every two months during treatment.
We are able to see on the scans if the pancreatic mass is shrinking; we can also assess tumor shrinkage with a blood test called CA 19-9.
If the tumor starts to shrink, we continue treatment for 4-6 months.
Sometimes radiation is added at the end of chemotherapy to sanitize the areas around the cancer margins and the lymph nodes.
After successfully finishing this treatment, patients proceed to surgery.
These patients who respond have the highest chance of getting to a successful surgery. These patients are also likely the least likely to have cancer recurrence.
For those patients who have cancer growth in other organs while on chemotherapy, we can avoid putting them through surgery because it is likely not going to help them. Most borderline resectable patients will also be able to have successful surgery with this approach.
For our patients who have stage 4 disease, surgery will not be an option. At this time, we can treat, but we cannot cure stage 4 pancreatic cancer. We treat them with chemotherapy. We offer them clinical trials. The goal of treatment is to prolong survival. We try to maintain quality of life during treatment with an emphasis on pain control, nutrition, emotional well being, mind-body techniques. We hope that the amazing advances in the treatment of other cancers like Melanoma and Lung Cancer will soon catch up to Pancreatic Cancer as well, and improve outcomes.
What is the role of Complementary and Alternative Therapies for Pancreatic Cancer?
That’s a great question.
In general, Complementary and Alternative therapies can be divided into 1. diets, supplements, and herbs; and 2. mind-body practices like yoga, meditation, acupuncture, hypnosis, massage, and Reiki
At our practice, we support and routinely offer therapies that are proven to be useful and are not going to interfere with treatments.
For example, meditation, yoga, and acupuncture help with anxiety, stress, and pain. Ginger helps with nausea control.
We need to be mindful of the fact that alternative therapy is not known to cure cancer. We encourage the use of CAM for “living well” through cancer treatment, rather than replacing cancer treatments.
Who should get screened for Pancreatic Cancer?
An ideal cancer screening method should be able to pick up all cancers and not miss any cancers. At the same time, it should not cause false alarms. Finding that method for Pancreatic Cancer has been elusive. That is one of the reasons Pancreatic Cancer screening has not been adopted at a population level.
At this time, we are recommending that individuals with high risk should undergo screening. Individuals with a high risk of Pancreatic Cancer like those with one affected family member with Pancreatic Cancer should be screened.
If someone has multiple affected family members with Breast Cancer or Ovarian Cancer or Melanoma, they should talk to someone to discuss screening.
If someone has a high-risk genetic mutation like BRCA 2, they should be screened.
A combination of imaging studies like Endoscopic US and MRI and blood tests like CA 19-9 can are commonly used for screening.
Do you recommend clinical trials to patients with Pancreatic Cancer?
Absolutely. We discuss the option of clinical trials with all our patients.
We are blessed to work with our colleagues at the Honor Health Research Institute who are doing wonderful work in the field.
These are ongoing trials looking at new experimental but promising drugs; or trying new combinations like immunotherapy with existing drugs.
What are some of the latest advances and future directions in the field of Pancreatic Cancer?
For Pancreatic Cancer, early detection is the key. My prediction is that blood-based testing for early detection of cancer will likely revolutionize cancer screening in the years to come. We have commercially available technology to detect cancer DNA in the blood. We are already using this technology in the clinics in the form of what we call a “Liquid Biopsy.” Currently, its use is limited to monitoring treatment for a few cancers; going forward, hopefully, we will be able to detect Pancreatic Cancer with a blood test.
It is believed that Pancreatic Cancer is hard to treat because Pancreatic Cancer cells are surrounded by a protective shell, called the stroma or micro-environment. There are ongoing trials that combine chemotherapy with drugs that degrade the stroma. The hope is to improve chemotherapy access to cancer cells.
There is also ongoing research aimed at harnessing the full benefit of immunotherapy in Pancreatic Cancer. Unlike some other cancers like Melanoma or Lung Cancer, immunotherapy has not had a significant impact on the treatment of Pancreatic Cancer. What remains to be seen is whether combining immunotherapy with chemotherapy drugs, or drugs that degrade the stroma around pancreatic cancer cells, will improve outcomes.
Acknowledgements: Dr. Albert Amini, at Arizona Premiere Surgery. Dave Pratt and Mark Lewis, at Star Worldwide Networks. Our awesome cancer care team at the Virginia G. Piper Cancer Care Network and Arizona Center for Cancer Care. Thank you all!


Recent Comments